It was like a Symphony…South Carolina Systems of Care! #twinslife #nicu
The morning started at 3:30am Saturday, June 10th being awaken by Sarah saying something is wrong. As I rubbed my eyes trying to figure out what was going on, I realized her swift movements to the bathroom indicated I better jump into action. As I ran into the bathroom, I looked at Sarah as tears ran down her face. I knew…I better call Dr. Hearn immediately. I wondered…how did this start.
We knew we wanted another child, and after Sarah had her last scare with a bad mammogram; we knew the window of time was closing on us. Her mother died of triple negative, metastatic breast cancer back in September 2007. Even though Sarah’s digital mammogram showed more slices and potentially more false positives…she knew she had to be proactive. She researched breast reduction and found Dr. Felice Moody at AnMed Health who performed the double breast reduction, removing the questionable tissue and significantly reducing her chances of breast cancer. She was thirty-eight when she had the surgery and knew after she recovered was ready for the next phase, trying to have a second child.
We knew the risks of getting pregnant at thirty-eight, we had done our research. Working in healthcare communications and advocacy, I was surrounded by the best and the brightest. I have spent the better part of 10 years working with large, medium and small health systems, health care trade associations and advocacy groups, and foundations that supported access to quality health care. These resources became a powerful backbone to many of our future decisions. I grew up in health care with my mom putting herself through nursing school when I was finishing high school, then she finished her MSN to become a Nurse Practitioner when I was in graduate school. I remember being a kid sometimes spending the night in Greenville Health System’s Emergency Department while my mom pulled a 7pm-7am shift. Health care has been and will always be a part of my DNA.
Having a second child, we think!?
I remember getting the call from Sarah one fall morning, she told me she was ready to call Dr. Nichols. Piedmont Reproductive Endocrinology Group (PREG) helped us figure out how to make the miscarriages stop and then our first miracle arrived, Rose Frances Rettew. Dr. Nichols was the doctor that helped us the first time, now it was time to talk about having a second child. She scheduled a visit for a Friday morning and was excited to put her surgery behind her and start planning for the next stage of our families future.
That Friday morning, she called me again with a proposition. She had learned that she had four eggs ready to go…Dr. Nichols told her to bring me early the next morning. We were going to try intrauterine insemination (IUI). I remember a nurse walking me back to the “weird room” and I asked her if this was a bit strange, I know i felt weird. She laughed and told me that her job was to take what I capture in a cup and bring life into the world; we laughed and then proceeded to talk about college football. After leaving the office that morning, I knew we were pregnant.
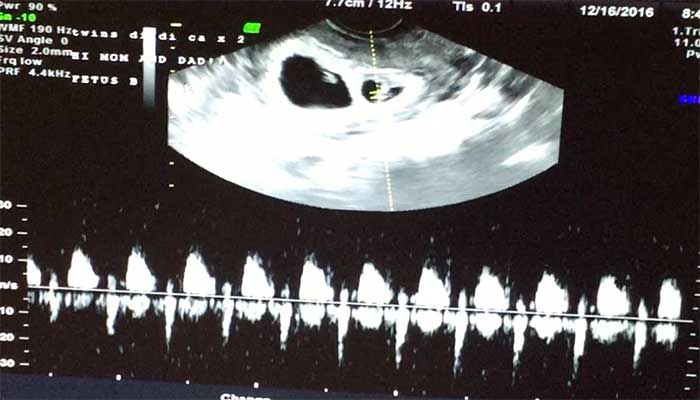
A few weeks later, on December 16th we found out we were having twins. Twenty days before Sarah’s 39th birthday, we watched the ultrasound at PREG in Greenville, SC showing us two little heartbeats that would change our lives. Twins. Our next visit was with Sarah’s most trusted doctor, her OB, Dr. Henry Hearn. Dr. Hearn had delivered Sarah’s youngest sister, her other’s sister’s three children, and Rose. A man that has delivered over 10,000 babies was the doctor Sarah needed to comfort her, to tell her that she was having twins and that everything was going to be ok. During that visit, a week after seeing the initial ultrasound he held her hand to comfort her, providing that crucial reassurance all husbands want their spouses to feel. He also told us we needed to have another set of physicians be a part of this experience. The Maternal Fetal Medicine (MFM) specialist of Greenville Health System, located next door to Dr. Hearn’s office at the North Campus of AnMed Health.
Both AnMed Health and Greenville Health System are my clients, along with the South Carolina Hospital Association. I knew the competitive nature of healthcare. I also knew the power of having Dr. Hearn right next door to the MFM. Two systems of care under one roof proved vital to this process of having twins. Throughout the pregnancy, both Dr. Hearn of AnMed and the physicians at GHS Maternal Fetal Medicine walked us though each stage of having twins. Sarah was considered high-risk given her age and the fact she was having twins. Both teams consistently monitored her progress leveraging newly implemented EPIC EMR, so they both could read Sarah’s chart’s in real time. I knew the importance of the connectively between EMR’s based on my work with Health Sciences South Carolina and the early stages of the SCHIEx with the health information exchange. This EMR connectivity would continue to be crucial during and after the pregnancy.
It was Wednesday morning, June 7th and Sarah was 32 weeks and three days. George and Henry were growing and it was time for a visit to see the GHS MFM’s. As we sat in the ultrasound, we were told that Henry was two pounds bigger than George. George was Baby A and his head was pushing down on Sarah’s cervix. Well, actually we learned that Sarah had a complete placenta previa, where Baby A’s placenta completely covered her cervix. It was confirmed that we would have a c-section, and they were moving up her scheduled delivery to the 36th week. We went home excited, George and Henry are might come home sooner rather than later. We had no idea what we were wishing for might actually happen.
The next morning about 5am, she woke me up saying she was bleeding. We rushed to AnMed Health. Dr. Hearn told us if this happened to come directly to the Women’s and Children’s wing of AnMed’s North Campus to see him. We spent the night in the hospital thinking everything was ok. During our 30 hour stay, she received the crucial steroid shots so the baby’s lungs could start developing faster. We went home on Friday thinking…we are in the home stretch. Little did we know what would happen next.
The Next Morning, June 10th – “It’s My Birthday”
After being woken by Sarah Saturday morning, it was like a broken record. Here we go again. This time, it seemed more serious. Sarah is sitting in the bathroom crying, while I am talking to Dr. Hearn on his cell phone at 3:30am. He told me to pack Sarah up and take her to GHS. Sarah did not want to go to GHS, she wanted Dr. Hearn to deliver George and Henry. She called him back and asked him why.
Dr. Hearn is more than a doctor, a physician, an OB. He is a friend, a trusted soul, a man that knows how to talk to his mothers. He knows what to say, how to say it, and how to listen. He gives out his personal cell phone. He accepts our calls at 3:30am. He just cares. He loves his patients, his mothers, his babies!
In his kind, soft voice; he explain to Sarah that if we came to AnMed Health, he would probably have to deliver the twins then send them to GHS’s NICU and keep her in Anderson to recover from the c-section. He told her that if she went to GHS and had to deliver the twins, everyone would be in one place to get the very best care we needed. I knew Dr. Hearn wanted to deliver the twins. I knew Sarah wanted to see him after they were born. I also knew Dr. Hearn put the patient(s) first.
I have worked with so many different systems of care. I have worked with advocacy groups supporting health care initiatives for low-income patients. I written video scripts and campaigns surrounding patient safety and surgical safety checklists; interviewed Dr. Atul Gawande, interviewed Helen Haskell mother of Lewis Blackman, and the list goes on and on. I have seen the big picture of health care all the way down to the granular, daily conversations of reimbursements, evidence based medicine, marketing campaigns to put heads in beds, and the importance of washing your hands. But, I never thought I would witness all these systems of care in one situation.
After rushing to GHS at 4:30am, I knew something big was going to happen. I hoped the boys could hold on a few more weeks, but a I had a weary feeling in my gut. As I raced Sarah down I-85 to GHS, I called my mother who spent 28 years in the GHS Emergency Department. She told me where to park and how to find OB Triage.
After rushing to the sixth floor and into OB Triage, I knew we were in a teaching hospital. Teams of physicians and nurses surrounded us, checking Sarah, checking the boys, telling us to prepare for a long day. Then it came…it was finally said…we were going to deliver. They had already read her chart and background, Dr. Hearn had called them to share the history as they reviewed her electronic medical records via EPIC.
As they prepped Sarah for surgery, I dropped into execution mode calling all the family, friends, ministers, and even Dr. Hearn. I told him what was happening, he re-assured me we made the right decision. I stood in the labor and delivery recovery room as they took her away. I watched my wife, my twin boys, my whole life and being wheeled away to surgery. My heart sunk!
The delivery room
I remember the orderly bringing me scrubs so I could get ready to join Sarah for the delivery. As I put them on and as the orderly helped me put on my mask, he stopped me for a second. He told me that on the other side of the door were 25-30 people preparing to deliver the twins. He told me it was going to be visually overwhelming. He told me my job was to sit with Sarah and talk to her through the whole process. I began to shiver and then found peace in his voice as he helped me open the door.
As I walked through the door, my eyes could not comprehend what I witnessed, 25-30 people working calmly, surrounding Sarah. I remember stopping and scanning the room. I noticed two NICU teams waiting for the boys. I noticed a surgical team on the other side of the sheet working on Sarah. I noticed Sarah’s face with that scared look I had seen before. But for a moment, something changed. I noticed the surgical safety checklist hanging on the wall. I watched each person wash their hands over and over before entering the surgical suite. I found comfort in these iconic pieces from my health care knowledge base. So many systems of care in one one situation. So many context’s from the years of work surrounding me in this one very moment. As I was stood in that doorway, I watched both my personal and professional life come to a complete standstill, contextualized in one very moment. It was as if I was at the very apex of my graduate oral defense, bring everything I learned to one argument in time. I found my confidence, a peace that would ultimately allow me to be a father in that operating room.
As each baby was being delivered, I was finding joy in each cry, each smile, each part of that delivery process. I was breathing the complete breath of life, knowing that everything was under control.
After the boys were born, I was whisked away to the NICU leaving Sarah behind. As we made our way to our little wing of NICU Level 1, it was time for me to sign numerous documents, allowing care to be administered to George and Henry. There it was, the Lewis Blackman Patient Safety form for me to sign for both George and Henry. It basically states that I understand the general roles of all clinical trainees, medical students, and resident physicians providing care to both George and Henry. As I signed, I thought about Helen Haskell. I thought about the numerous interviews I had with her, digging deep into her story, her son’s story, and the true meaning of the Lewis Blackman Patient Safety Act. I looked up at the nurse holding these forms, looking at her name badge, thinking about this one piece of legislation is the reason why she is wearing that badge today. I was able to somewhat contextualize those tears in Helen’s face each time she speaks during the annual patient safety awards at the Transforming Health Symposium. I thought, I wish Helen could be here right now to witness this moment.
“It was like a symphony!”
A few years ago, I had the great privilege to tell an amazing story about an amazing man who survived a heart attack, all because the numerous systems of care worked together to save his life. Mr. Johnny Fields had a heart attacked in rural Oconee County, South Carolina. At the time, Oconee Memorial Hospital was not a part of Greenville Health System, yet all the first responders worked seamlessly to get him to Greenville Memorial Hospital is 63 minutes to save his life. He described all these people working together to save his life using the metaphor, it was like a symphony.
Yes it was…it was like a symphony. All the instruments, all the musicians came together in perfect symphonic motion and saved Mr. Johnny Fields’ life. Our story is like a symphony, so many pieces to this puzzle, so many parts…and it amazes me that this happens everyday.
George and Henry are doing well, gaining weight and learning now home from the NICU at Greenville Health System. Sarah recovered well from the c-section and is learning the new normal as we balance life with twins in the NICU and after the NICU, along with our five year old daughter needing our attention. It is these systems of care working together like a symphony, that made this possible. It is these systems of care bring new innovations to the hospitals of South Carolina everyday. It is these systems of care that provided my mother a long career, put food on the table when I was young man and now as I grow my own family, provides the very resources to raise that family. I am thankful for the work I do everyday representing numerous hospitals in South Carolina. These very systems I advocate for each day, provided the necessary care for the family I love. I am thankful.




A great story with a happy ending. Thank you for sharing Bobby.
John…I was super happy to see you reading this post. I have found so many intersections between serving hospitals in South Carolina and finding my family in the patient role. This experience has been the hardest challenged I faced to date…it has stretched me in so many ways. It is my hope that my words help others, including other dads, know that there is no such thing as normal in the world of twins, NICU, healthcare, and trying to keep a business rolling. Thanks so much for your support!